In ageing societies, back problems have become a widespread debilitating condition. In many cases, the underlying cause is spinal canal stenosis. Bony constrictions form in the spinal canal, which press on the spinal cord. Chronic pain and signs of paralysis are the result. In around 111,000 cases in Germany alone, they become so severe that only surgical decompression of the spinal canal can help. Surgeons use high-speed cutters to open up the spinal canal to remove the constrictions that are growing inside.
Risky procedure on the spinal canal
Such procedures are challenging for the surgeons. While milling requires high contact pressure and thus physical strength, the close proximity to the spinal cord and nerve roots requires dexterity. In 1.5 percent of operations, the high-speed rotating milling head nevertheless comes into contact with the nerve tracts. In this case, those affected are at risk of bladder and rectal incontinence or paraplegia. In addition to personal suffering and loss of life quality for those treated, such catastrophic surgical procedures are associated with psychological stress for the medical teams and considerable follow-up costs for the healthcare system.
To minimize the risks of surgeries near critical neuronal structures, a research team led by Dr. Achim Lenenbach, head of the Laser Medical Technology and Biophotonics Department at the Fraunhofer ILT, is driving forward robotically assisted laser surgery systems. A solution for gentle skull opening for neurosurgical procedures is already well advanced. Here, a short-pulse laser replaces the milling machine. In addition, the cutting depth is continuously measured using optical coherence tomography (OCT). “We intend to use this approach for surgical procedures on the spine in the future,” he explains. A patent application has already been filed for the idea of a robotically assisted laser surgery system for the precise and safe cutting of bones.
Short-pulse laser and OCT measurements for precise hard tissue cuts
The principle of such laser surgery systems is based on ablating the bone tissue with nanosecond laser pulses. The short pulse duration not only has the advantage of minimal thermal interaction with the surrounding material, which prevents carbonization of the cut edges and promotes the healing process, but also ensures a high degree of microsurgical precision. This is because a local thermomechanical effect only occurs where the infrared laser pulses hit the hard tissue: The water stored in the bone vaporizes explosively and creates micro-craters in the bone.
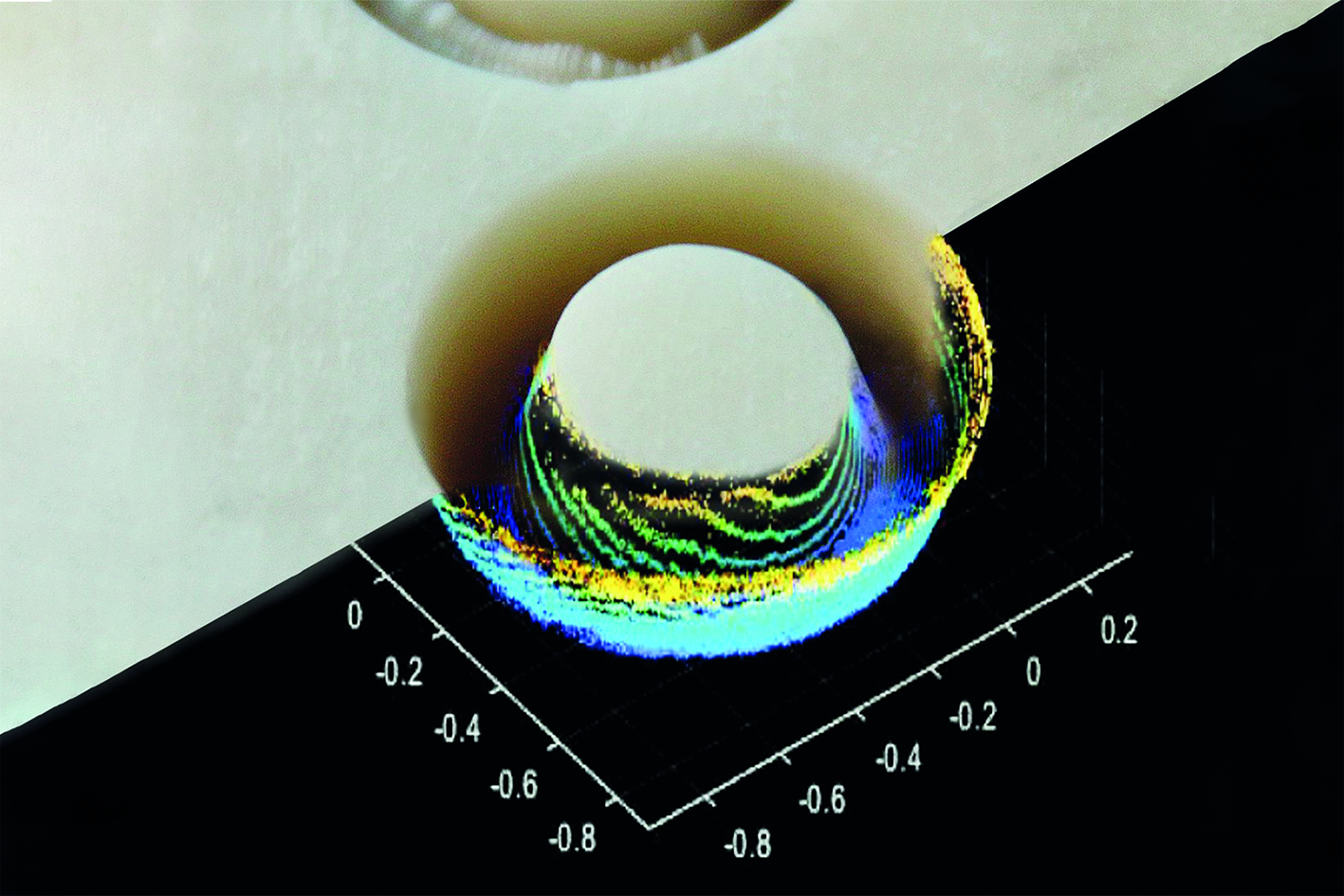
To achieve the ablation rates required in surgical practice in a gentle cutting process, a spray mist system moistens the surface of the bone while a galvo scanner guides the laser focus along the intended cutting line. This also reduces the thermal stress on the surrounding tissue. For use in spinal canal operations, it is also essential to monitor the cutting process. For this purpose, the cutting laser beam is superimposed with an OCT measurement beam which the scanner also guides over the bone surface. The system detects the cutting area in three dimensions: the beam penetrates the bone tissue and can determine the thickness of the remaining bone lamella at the bottom of the kerf from a residual thickness of approximately 400 µm. The OCT measurement carried out synchronously with the cutting process is therefore the key to reliable - and highly safety-relevant - control of the cutting process based on the residual bone thickness. Once the individually defined residual thickness has been reached, the cutting process should stop automatically. The surgeons can then lift off the loosened bone with little effort and without risk to the nerve tracts in the spinal canal.
High technology for safe medical care
“Based on the scheduled optical monitoring and precise control of the laser cutting process, our procedure could prevent serious injuries to the spinal cord and nerve roots in future,” explains Lenenbach. At the same time, the use of the system is expected to minimize complications that often unnecessarily prolong hospital stays after spinal canal stenosis operations.
For spinal operations, the Fraunhofer researchers are planning a further development of their existing applicator, which is designed for operations on the head. This contains the optical functional elements such as the scanner and optical lenses and guides the focused cutting laser and OCT measuring radiation along the incision line. This applicator now needs to be miniaturized and designed as an ergonomic handpiece so that surgeons can also carry out the currently automated cutting process manually. The surgeon is to be supported by a collaborative robotic system for precise manual guidance of the applicator. The research team is also planning to address another previously unsolved problem during further development: While a milling cutter has direct contact with the bone and provides surgeons with direct haptic feedback, this feedback must be provided via a detour in the non-contact laser cutting process. The researchers are planning to use the sensors and actuators of a collaborative robot (cobot) for this purpose. This is because the cobot's force-torque sensor system determines the force effect on the robot arm, which the actuator system can then use to provide the operator with haptic feedback when manually guiding the laser applicator.
If the haptic feedback of the cobot is combined with the OCT sensor technology, the feed of the handpiece can be controlled by the surgeon based on the force effect so that it only takes place when the cutting process has locally reached the defined residual thickness. Iteration of the local microcut and feed, combined with efficient hard tissue removal, will result in a quasi-continuous cutting process.
Haptic and visual feedback for surgeons
In addition to haptic feedback, the surgeon's visual orientation is crucial for the safety of semi-automated laser surgery. The laser surgery system is therefore to be linked with surgical planning software and a navigation system. In such an integrated system, the laser-generated incisions can be visualized in real time in the preoperatively generated image data. Surgeons could follow on the monitor how deep their incision has already penetrated the bone and how close they are to neuronal risk structures. In the planned research project, the development of the surgical planning and navigation software will be the responsibility of industry partners with proven expertise in this field. “The laser surgery system developed at our institute could implement the preoperatively planned incisions with sub-millimeter precision,” says Lenenbach.
The long-term research goal is to establish robotically assisted laser procedures for cutting hard tissue as the gold standard for operations close to critical structures. This could relieve hundreds of thousands of patients from the fear of the consequences of spinal cord injuries during such operations, which become a bitter reality for thousands of patients worldwide every year.
 Fraunhofer Institute for Laser Technology ILT
Fraunhofer Institute for Laser Technology ILT